Sleep apnea is one of human kind’s major health problems. It is estimated that 20% of the human population is affected by sleep apnea. Apnea causes poor sleep quality, decreased quality of life, chronic medical conditions, and early death. If you or a loved one suffers from sleep apnea, you should know and understand as much about it as possible. The following pages are available to give you important information about the disorder and its treatment.
SLEEP APNEA – WHAT IS IT?
Sleep Apnea Syndrome is the result of changes in breathing during sleep. These changes, or events, must happen with a certain frequency in order for the condition to be present. To learn more about what is happening during an apnea event, the causes of sleep apnea, and how we measure apnea events, visit the page, What is it?
SLEEP APNEA EVALUATIONS
Do you wonder if you have sleep apnea? Do you know whether or not you should be evaluated for it? What tests are required to determine if you have apnea during sleep? Can testing be done at home? For answers to these questions, visit the Evaluations page.
SLEEP APNEA TREATMENT
Have you been diagnosed with Obstructive Sleep Apnea? Are you wondering what to do now? Do you want to know more about the treatment options available to you? The Treatments page serves as a general guide to the various treatments currently available. It is important to discuss each option with your healthcare provider or sleep specialist to make sure the option you choose is the right one for you.
POSITIVE AIRWAY PRESSURE TREATMENT AND EQUIPMENT
Most people with moderate to severe Obstructive Sleep Apnea use some form of positive airway pressure to correct the problem. The most common form is constant positive airway pressure, or CPAP, but there are other types of pressure machines and treatments. The various means of treating sleep apnea are reviewed on the Equipment page.
What is it?
OBSTRUCTIVE SLEEP APNEA SYNDROME, WHAT IS IT?
Sleep apnea is a very common problem. It is a breathing problem that occurs during sleep. Several types of apnea problems have been recognized, but by far the most common is Obstructive Sleep Apnea. It accounts for over ninety-five percent of the individuals who have problems with sleep apnea.
What is apnea? What is obstructive apnea? What does it do? Anyone who has been diagnosed with sleep apnea or has a loved one with sleep apnea should know the answers to these questions. Apnea occurs when breathing stops. Obstructive apnea happens frequently when breathing stops because of obstruction of the airway.
The medical problem – Obstructive Sleep Apnea – is a syndrome. A syndrome is a grouping of signs, symptoms and findings, which when placed together, are considered to be a medical condition. Syndromes are usually diagnosed by a person’s symptoms, physical findings and laboratory abnormalities. The Obstructive Sleep Apnea Syndrome is a combination of varying degrees of sleep symptoms, sleep test abnormalities and to a lesser degree, abnormalities in the physical examination. Apnea events interrupt sleep and symptoms result, but apnea is much more than symptoms. There are long-term consequences.
THE EVENTS
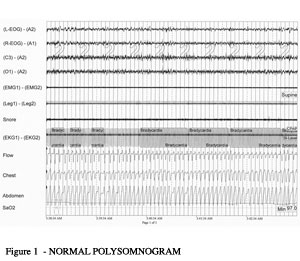
Apnea means “no breath.” When people have sleep apnea problems they are suffering from interruptions in their breathing while asleep. With the obstructive sleep apnea syndrome, the interruptions in breathing occur when the airway becomes blocked during sleep. The chest and diaphragm are making efforts to pull air into the lungs, but the passageway to the lungs is blocked. Figure 1 shows a five-minute tracing of a normal sleep test. It shows a snoring microphone recording (no snoring is seen on this record), electrocardiogram, flow of air through the nose and mouth, chest and abdominal wall movements, and the level of oxygen saturation.
FIGURE 1 – NORMAL BREATHING DURING SLEEP
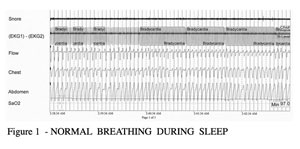
FIGURE 2 – SLEEP APNEA DURING SLEEP
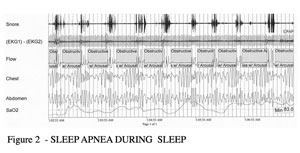
Figure 2 shows five minutes of severe sleep apnea. Note the loud snoring, the absence of airflow (shaded areas on the flow channel), changes in respiratory effort in the chest and abdomen, and the changing oxygen levels.
Breathing is an act that we do not have to think about. It occurs regularly, without conscious thought and is regulated by physiologic factors. We breathe when we do because of the controls built into our body’s respiratory system. The levels of oxygen and carbon dioxide in our blood, the sensations of our muscles in the chest and diaphragm and the amount of acid in the blood, are all factors that determine the depth and frequency of our breaths. During sleep, our breathing is under the same controlling factors. When obstruction to the airway occurs, the sensors that control our breathing note that change and then cause an increase in the physical effort to breathe. As a result of the effort, air begins to move again.
These obstructive events occur over and over again. As seen in Figure Two in someone with the obstructive sleep apnea syndrome, they occur many times per hour. The events can result in total blockage of the airway (apnea), partial obstruction of the airway (hypopnea), or a lesser degree of obstruction (airflow reductions with arousal). These events have varying effects on the person who has them.
THE SYMPTOMS
The majority of complaints from patients with obstructive sleep apnea syndrome focus on the quality of sleep. The person frequently does not sleep well, often has non-refreshing sleep and complains of daytime sleepiness. Almost any symptom related to the quality of sleep or the ability to sleep may be reported. Frequently reported symptoms are listed in Table 1.
|
SYMPTOMS OF OBSTRUCTIVE SLEEP APNEA
>
|
WHAT CAUSES OBSTRUCTIVE SLEEP APNEA?
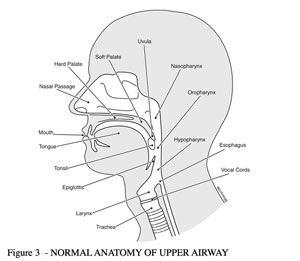
The obstruction of the airway that causes the syndrome is reversible. In fact, it comes and goes. It occurs only during sleep, usually in individuals who have little awareness of the events. While awake these individuals breathe without problems. While the reason obstruction occurs remains under research, physicians now know a great deal about the site of the obstruction and individuals who develop obstructive sleep apnea.The site of the obstruction occurs in the upper airway. That is the area above the larynx (voice box). The larynx and the airway below are held open by rings of cartilage and do not collapse. However, above the larynx the reversible obstruction occurs at the base of the tongue or at the soft palate. People with obstructive sleep apnea are essentially choking in their sleep.Figure 3 shows the normal anatomy of the upper airway. The obstruction in sleep apnea occurs above the larynx.
FIGURE 3 – NORMAL ANATOMY OF THE UPPER AIRWAY
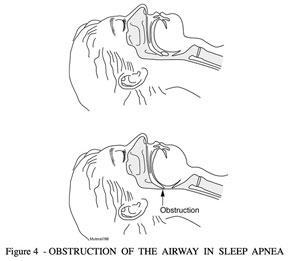
Physicians have a good idea of the mechanism that results in the obstruction. The vast majority of individuals have no abnormalities of their airways. Their throats show normal tissue in normal places. For a great deal of time it was thought that a specific reason for the apneas would be discovered. However, that has not been the case. A few individuals have significant and obvious problems in their airways: enlarged tonsils, enlarged adenoids, growths or birth defects in their jaw area. These abnormalities result in a small upper airway that obstructs easily upon reclining. Uncommonly, severe hypothyroid problems result in obstructive sleep apnea.The reversible obstructions occur mostly in normal throats. Over the past thirty years doctors have investigated why the obstructions occur and how they occur. It is clear that a large number of overweight people have obstructive sleep apnea. It has been found that when morbidly obese individuals with sleep apnea lose weight, the obstructive sleep apnea will go away about fifty-percent of the time.Thin people have obstructive sleep apnea, too. Men, women and children have obstructive sleep apnea. They may be tall, short, thin or stocky. Studies have shown that five to fifteen percent of the American population has some degree of obstructive sleep apnea. After studying thinner individuals and obese patients who still have obstructive sleep apnea after weight loss, medical specialists are beginning to come to the conclusion that there are two major factors that result in the obstructions. The two factors are: 1) the degree of muscle relaxation that occurs in the upper airway muscles during sleep and 2) the size and shape of the throat.Figure 4 demonstrates the site of obstruction for the majority of patients with the obstructive sleep apnea syndrome. The arrow shows the area where the palate and tongue obstruct the airway during sleep.
FIGURE 4 – OBSTRUCTION OF THE AIRWAY IN SLEEP
APNEA – WHAT DOES OBSTRUCTIVE SLEEP APNEA DO?
The obstructive events have two major effects. First, the events cause a disruption in the sleeping patterns of the brain and second, the events place a stress on the cardiovascular system. When the obstructions occur, the brain senses that the breathing is not effective and breathing efforts are increased. The effort needed to open the obstruction can awaken the sleeper, or at least cause the person to change to a lighter stage of sleep. These events result in release of stress hormones, changes in heart rate, changes in blood pressure, a drop in the blood oxygen level and other changes.Apnea will ruin a night’s sleep. People perceive that sleep is a quiet, inactive time. However, sleep is a very active time for the brain. Imaging studies demonstrate that during sleep the brain functions at a high level in a rhythmic pattern. It could be interpreted as ‘when we sleep, the brain works and the body rests’. The obstruction of the airway, disrupts the rhythmic pattern of the brain during sleep. This pattern will be restarted over and over again, but the obstructive events interrupt the processes. A few individuals will wake when the obstructions occurs, but most will have no idea what is happening. They will complain of a bad night, feel like they haven’t slept or feel sleepy during the day. It affects each person differently, but for everyone, sleep is disturbed at some level by the obstructive events and symptoms usually follow. Symptoms and patients’ comments are listed in Table 1 above.
The second effect of obstructed breathing is on the cardiovascular system. When an obstruction occurs, it results in a release of catecholamines (adrenal stress hormones) and changes in blood pressure and heart rate. The oxygen level drops repeatedly, often to dangerously low levels. Individuals with the Obstructive Sleep Apnea Syndrome suffer these events repeatedly night after night, week after week, and year after year. The cumulative effect results in medical problems. Patients with sleep apnea have higher rates of elevated cholesterol, diabetes, high blood pressure, heart attacks, and strokes. Patients with a high number of obstructive events die significantly younger than those who do not have apnea problems. Many other medical conditions are also thought to occur more frequently when apnea is present.
HOW IS THE SEVERITY OF OBSTRUCTIVE SLEEP APNEA MEASURED?
The number of significant obstructive events that occur per hour measures the severity of obstructive sleep apnea. The events are reported as the apnea/hypopnea index (AHI). Symptoms usually are more frequent and intense as the AHI increases. Essentially all insurance companies use the AHI to indicate the presence of obstructive sleep apnea and rate its severity. Medical studies have confirmed that the long-term complications associated with obstructive sleep apnea do increase as the number of events per hour increases.
The higher the AHI measured during a sleep test, the greater the risk of medical complications. It has been demonstrated that an AHI of less than five has no long-term risk. However, an AHI of greater than thirty predicts a very high risk of developing problems. Obstructive sleep apnea is rated: AHI of five to fourteen – mild, AHI of fifteen to thirty – moderate, and AHI of greater than thirty – severe.
Other sleep test measurements also influence the reviewing physician. Individuals who show very long apneas (thirty to ninety seconds), very low blood oxygen levels and heart rhythm disturbances with the apneas, may be considered to have severe obstructive sleep apnea even when the AHI is only mildly or moderately increased. In addition, patients have been recognized who have symptoms of obstructive sleep apnea even when the AHI is less than five. These patients’ symptoms usually resolve on positive airway pressure therapy.
Evaluations
EVALUATION FOR OBSTRUCTIVE SLEEP APNEA
Sleep is a very personal time. We are unaware of our surroundings and are unprotected. We don’t know if we move, talk or snore. We are unable to present the best image of ourselves. We are vulnerable and helpless. Those we let into our personal lives, family, friends and loved ones, may tell us things about what we do during sleep, things we do not believe. Other times, we experience things that our loved ones do not see or have trouble believing. There may be no one to tell us if we are doing something unusual during our sleep.
Many of us are reluctant to seek help for sleep problems. We dislike having someone outside our inner circle involved in such a personal problem. In the past, it was not unusual for physicians to tell patients that a sleep problem was all in their heads. Now, the medical profession is more enlightened and knowledgeable. There are professionals who specialize in sleep problems.
This section is designed to help you answer questions you may have regarding the evaluation of sleep. Who should be evaluated? Who should do the evaluation? What kinds of tests are performed? Where should the tests be performed?
WHO SHOULD BE EVALUATED?
Absolute Indications for a Sleep Evaluation
Anyone who has symptoms or signs that suggest sleep apnea should discuss them with their physician. There are a few things that are absolute indicators of the need for a thorough evaluation – sleep testing. So how do you decide? When is your complaint an indicator of a serious medical condition?
Let’s start with the absolute indicators: those things that strongly suggest the presence of a significant breathing problem during sleep. The first is loud snoring. A sleep evaluation and testing are indicated if your snoring ‘rattles the rafters’, ‘shakes the walls’, can be heard at the other end of the house, is loud enough that it is easily heard outside the room or consistently drives your mate to another room to sleep.
If you are observed to have periods during your sleep when your breathing is seen to stop, sleep evaluation and testing are indicated. While normal individuals can have an occasional obstructive event associated with cession of breathing, repeated observations strongly indicate a problem.
If you are extremely sleepy, sleep evaluation and testing are indicated. Normal individuals sleep eight to nine hours a night and feel rested. It is abnormal to sleep ten to twelve hours and be sleepy during the waking hours. Sleeping more than ten hours a day means you should seek help. If you are sleeping seven to eight hours per night and falling asleep during normal activities, you should seek help. Falling asleep while doing dangerous activities such as driving or working with machinery is an absolute indication that sleep evaluation and testing are indicated.
When someone exhibits more than one of these three absolute indicators – loud snoring, observed cessation of breathing during sleep and excessive sleepiness – the question is not, “Does that person have apnea?” but, “How bad is it?” However, most people who suffer from significant obstructive sleep apnea, even many of those with severe apnea, do not report such extreme symptoms.
Symptoms of Obstructive Sleep Apnea
The symptoms of obstructive sleep apnea are primarily those of disturbed sleep, excessive sleepiness and non-refreshing sleep. Unfortunately, there is not one specific symptom to identify individuals with obstructive sleep apnea syndrome. Common symptoms are listed in Table One. If you are experiencing one or more of these symptoms, speak to your physician. A sleep evaluation and testing may be indicated.
|
SYMPTOMS OF OBSTRUCTIVE SLEEP APNEA
>
|
SELF ASSESSMENT
Take the sleep quiz on this web site. It is another way of determining if you might have the syndrome. The Epworth scale can give you some insight as to the importance of your daytime symptoms. It can indicate sleep problems and suggest whether a sleep evaluation is needed. Both of these quizzes can help you decide if you should seek further advice and evaluation.
TESTING FOR OBSTRUCTIVE SLEEP APNEA SYNDROME
The only way to know if you have the syndrome is to be tested. A formal sleep test (polysomnogram) performed in a sleep center is the only way to be absolutely sure of what happens when you sleep. It is the test required by insurance companies to verify that a person has obstructive sleep apnea.
POLYSOMNOGRAM
A sleep test (polysomnogram) measures sleep duration and stages, breathing, blood oxygen saturation, electrocardiogram, muscle contractions and body movements. It is a non-invasive test. All the sensors are strapped on or attached with adhesive material. A polysomnogram is a highly complex series of measurements. It is the only test that can answer the question: “Do I have sleep apnea?”
Many things are measured during a polysomnogram. The tests included are an electroencephalogram (EEG), electromyograms of chins and legs (EMG), electro-oculogram (EOG), electrocardiogram (ECG), airflow through the nose and mouth, chest and abdominal movements, limb movements, blood oxygen saturation and body position. For the electroencephalogram (EEG), a measurement of brain waves, eight to ten electrodes are glued to the head and scalp. The EEG, EMG and EOG demonstrate a characteristic pattern during sleep allowing a determination of the depth of sleep. The electromyogram is a measurement of muscle tone. The electro-oculogram records the movement of the eyes. These three tests, the EEG, the EOG, and the chin EMG are used to define sleep.
Breathing measurements are made from airflow, chest and abdominal wall movements, and the blood oxygen level sensor recordings. Air movement through the nose and mouth is measured with a sensor worn under the nose, much like the tubing used to give oxygen to a sick person. The chest and abdominal wall movements are recorded from elastic belts worn around the chest and abdomen.
The remaining recordings measure changes that may result from apnea or may occur independently of apnea. Body movements during sleep occur very commonly. They may be a problem for the person who has them, they may just be an observation without significant effects to the person, or they may be the result of sleep apnea. The visual monitoring of the person while sleep adds information regarding the nature of the movements that occur.
A recording from a polysomnogram during a normal period of sleep is shown in Figure 1.
FIGURE 1 – NORMAL POLYSOMNOGRAM
Each type of measurement performed on a polysomnogram requires special knowledge of the test. Often, a specially trained technician carries out each type of test. However, a polysomnogram technician (sleep technician) must be skilled in multiple physiologic testing tasks. It is very important that properly trained technicians perform the test.
Polysomnograms are performed in specialized testing centers. The American Academy of Sleep Medicine, the organization of physicians and interested medical professionals, has set standards for sleep testing centers. The standards define the training requirements for the personnel, the procedure for the testing techniques, the physical requirements of the facility and appropriate working hours and responsibilities for the staff. In short, the Academy defines what is required to perform the testing in an appropriate manner. The Academy has a program to accredit sleep centers and sets very high standards. The best way to be sure that you have a sleep study of good quality is to be tested at a sleep center accredited by the American Academy of Sleep Medicine.
OTHER TESTING
Are there alternatives to the polysomnography test for sleep apnea? The American Academy of Sleep Medicine, Medicare and essentially all health insurance companies require a polysomnogram performed in a sleep center for the diagnosis of Sleep Apnea Syndrome. Several testing techniques are used to screen for the problem. If an abnormal result is obtained, a polysomnogram is usually required. The most commonly used screening test is an overnight oximetry.
OXIMETRY TESTING
Oximetry testing is a widely available technique. It is used to determine the oxygen level in a person’s blood. A small sensor with a red light is attached to the finger and the oxygen saturation is determined. It is the same sensor used during the polysomnogram. The oximetry-testing unit has a memory and records the blood oxygen level during sleep. Changes in the oxygen level can suggest, but not diagnose, sleep apnea.
HOME SLEEP TESTING
There are a number of commercially available home testing systems. Since insurance does not pay for home sleep tests, no particular test is widely used.
WHERE DO YOU GET HELP?
People frequently ask how to select a sleep physician or a sleep center that can provide advice and help. As always, the informed person is the wise consumer. Ask your physician. Ask friends and colleagues. Check out reference sources. Sleep physicians in each state are listed on the American Board of Sleep Medicine’s web site. Most states have web sites that list local sleep physicians and their qualifications.
Sleep testing can be found in many locations owned by physicians, hospitals and business companies. How do you find a center that has demonstrated a high quality track record? Centers accredited by the American Academy of Sleep Medicine meet the requirement. They are listed at the Academy’s web site.
If you have been recommended to a center, check to see if it is accredited by the Academy. Also, determine the ownership. Centers owned and operated by physicians or hospitals are usually a good choice. Centers owned and operated by medical equipment companies and business entrepreneurs should be suspect. What should be of concern to the potential patient? Who is the physician responsible for the testing and the interpretation of the test? Is he a local specialist? Can he be seen if you need help with your sleep problem? See ‘What to Look For in a Sleep Center’ for more information.
Treatments
THE PROBLEM OF OBSTRUCTIVE SLEEP APNEA
Sleep apnea syndrome is caused by frequent reversible obstructions of the upper airway causing interruption of sleep. These obstructions have two effects on the person who has them. First, symptoms of disturbed sleep result from the interruptions. Treatment should improve the quality of sleep and reduce symptoms. Second, the obstructive events can cause long-term consequences. High blood pressure, heart attacks, strokes, diabetes and elevated cholesterol levels have all been associated with increased frequency of obstructive events. Treatment should also be able to prevent these problems. In fact, treatment of apnea, when it successfully eliminates the obstructive events, has been shown to achieve both of these goals.
How do we treat individuals with throat collapse and those with excessive body weight as they work to lose weight? The three traditional categories of treatment are medications, surgeries and medical devices. The miscellaneous causes of apnea are beyond the scope of this discussion.
| CAUSES OF OBSTRUCTIVE SLEEP APNEA SYNDROME | |
| Excessive Body Weight | 25% |
| Miscellaneous causes (Throat abnormalities, metabolic abnormalities, etc.) | <5% |
| Non-specific throat collapse | 70% |
WEIGHT LOSS
Under ‘Obstructive Sleep Apnea, What is It?’ the causes of sleep apnea were reviewed. Excessive body weight is seen in over half the patients diagnosed with sleep apnea syndrome. There is evidence that with weight loss the sleep apnea of about half of the overweight patients will disappear. Weight loss is strongly encouraged in all overweight individuals. It is the treatment most likely to result in a long-term resolution of the problem.
MEDICAL DEVICES
Positive Airway Pressure
The two types of medical devices used to treat obstructive sleep apnea are positive airway pressure and dental appliances. It has been known for over twenty years that obstructive sleep apnea can be corrected by positive airway pressure. When the air pressure in the throat is raised to slightly higher than the local atmospheric pressure, the throat does not collapse. When the throat does not collapse, the obstructive sleep apnea syndrome is corrected. The symptoms resolve and the risk of long-term complications are markedly reduced. With consistent use of positive airway pressure, the symptoms related to poor sleep are usually resolved and the long-term risk for elevated blood pressure, diabetes, elevated cholesterol, heart attack and stroke returns to that of the population without sleep apnea. Positive airway pressure is the primary therapy for all levels of obstructive sleep apnea. Positive airway pressure is a simple concept. The details of the treatment are covered under the Equipment tab above.
Dental Appliances
Dental appliances work by holding the lower jaw (mandible) forward. This holds the back of the tongue away from the back of the throat and at the same time pulls the palate forward. The appliances are effective in reducing obstructions, especially in individuals with lesser problems and may be of value in patients who suffer from milder levels of sleep apnea syndrome. Dental appliances are considered when therapy with positive airway pressure fails. If the obstructive events are low in number and the person’s symptoms are mild, a dental appliance may be effective.
MEDICATIONS
In the vast majority of patients with sleep apnea syndrome, throat collapse during sleep is the cause of the obstructive events. It appears that both the size and the shape of the throat, along with the relaxation of the pharyngeal muscle tone, determine if the throat will stay open or collapse during sleep. There are no known medications that increase the size of the throat or increase the muscle tone of the pharyngeal muscles. At present, there are no medications to prevent and treat sleep apnea.
SURGERIES
If abnormalities are discovered in the upper airway, then surgery may play a major role in the correction of obstructive sleep apnea. For example, removing enlarged tonsils that are obstructing the airway will often correct the apnea in those individuals.
For individuals who have no anatomic abnormalities, surgeries have been designed to treat their obstructive sleep apnea. All the procedures are designed to increase the size of the throat, either at the level of the palate or at the base of the tongue. A number of procedures have been described for both locations. The procedures have some general features in common. They are not used as the first treatment for obstructive sleep apnea. Generally, when used they are successful less than 50% of the time, are quite painful for two to three weeks afterward and have some associated long-term complications. There is a third type of surgery which is a major surgical procedure designed to enlarge the space behind both the palate and the tongue. In this procedure, both the upper jaw (maxilla) and lower jaw (mandible) are moved forward. Maxillo-mandible advancement is a technically demanding major surgical procedure which is only effective 70% of the time. Because of the low success rates, surgical therapies for obstructive sleep apnea are used when traditional therapy with positive airway pressure fails.
MEASUREMENT OF SUCCESS
Obstructive sleep apnea is treated to both eliminate symptoms and to eliminate the obstructive events. Symptoms that result from the problem should be resolved or improved. The obstructive events need to be eliminated. Correcting the AHI to a normal level ensures the reduction of long-term adverse events to a normal level. Any treatment chosen should achieve both goals. The success of treatment should be measured both by how you feel and what happens to the obstructive episodes while you sleep. How you feel will be clear to you, but the obstructive episodes will not always go away when symptoms improve after treatment.
To ensure that the obstructive events have disappeared, retesting is indicated after weight loss, after surgery to enlarge the airspace, and after dental appliances are properly fitted and used.
If the treatment is positive airway pressure, a sleep test while wearing the pressure mask is usually performed prior to beginning treatment. This ensures that the events are resolved and determines the appropriate pressure for home therapy. If not retested at the sleep center, a home test should be used to ensure that the events are resolved.
Equipment
CPAP THERAPY AND EQUIPMENT
The most effective and least invasive means of treating sleep apnea is with positive airway pressure (PAP). Positive airway pressure works by keeping the airway open while a person sleeps, allowing them to breathe properly. Positive airway pressure is the treatment of choice for all patients with moderate or severe sleep apnea and for most with mild but symptomatic obstructive sleep apnea.
Under the “WHAT IS IT?” tab above, we described what it is and how it affects a person who suffers from it. This portion of the site is designed to introduce the treatment of obstructive sleep apnea with positive airway pressure.
GOALS OF TREATMENT
The goals of treatment with positive airway pressure are to improve health and overall well-being. The specific objectives are to improve the quality of sleep and to reduce the number of apnea events to safe levels. Improved sleep quality usually alleviates the symptoms caused by sleep apnea. The most common symptoms of sleep apnea that improve are sleepiness and fatigue. However, PAP can also eliminate or at least improve other problems such as snoring, insomnia, lack of concentration, nighttime urination and frequent nighttime awakenings.
Treatment with PAP is known to lessen the risk of developing long-term health conditions such as hypertension, stroke, diabetes, elevated cholesterol and heart disease. Studies have shown that when the number of obstructive events are reduced to normal, the risk of these long-term complications returns to the risk of the general population without obstructive sleep apnea.
When PAP therapy has been recommended to you, remember that the objectives of treatment are to improve symptoms and to control the obstructive apnea events. PAP will improve symptoms most of the time (greater than eighty percent) and the obstructive events, almost all the time (greater than ninety-five percent).
HOW POSITIVE AIRWAY PRESSURE WORKS
Positive airway pressure is the most effective form of treatment for obstructive sleep apnea. PAP is almost universally effective at correcting the obstructive breathing events. Most sleep apnea is caused by the collapse of the throat when the muscles relax during sleep. When the air pressure in the throat is increased, collapse does not occur as the muscles relax. The pressure acts as a brace or stent and holds it open.
Positive airway pressure causes one to breathe air at a slightly higher pressure than that of room air. For the patient with sleep apnea, the pressure is usually kept at a constant level above normal atmospheric pressure. The pressurized air has to be held in place, contained by a mask of some type. To achieve this pressure, a machine forces air through a connecting tube into the mask. The masks are designed to continually leak air in a limited controlled amount. To maintain the pressure, air is forced into the system constantly. When the person inhales, the air pressure will start to drop. Then the machine will sense the change and increase the air it forces through the system to maintain the pressure at the constant level.
There are different types of air pressure systems used to treat apnea. In each system the general concepts are the same. The air pressure at the mask is set and maintained by the machine pumping air into the system. Most of the time it is constant, however, modern technology has developed equipment capable of adjusting pressures automatically.
COMPONENTS OF POSITIVE AIRWAY PRESSURE THERAPY
There are several components involved in positive airway pressure therapy: A pressure source, a humidification source, a form of interface (mask) and tubing to connect the system. The system is designed to create a small world of carefully controlled, elevated air pressure for you to breathe.
PRESSURE SOURCES
The most commonly used form of pressure source is called CPAP, or Constant Positive Airway Pressure. As its name suggests, a CPAP machine delivers a single, constant level of pressure to keep the airway open. The person using CPAP will inhale and exhale at the same pressure. Most CPAP machines can be set as low as 4cm of pressure or as high as 20cm. The amount of pressure needed to keep an airway open is usually determined during a sleep study where the positive airway pressure is gradually adjusted to a level that controls the obstructive events.
The second common pressure source is Bi-level. A Bi-level machine delivers two set levels of positive pressures. A higher pressure is delivered during inhalation, and a lower pressure during exhalation. When relatively high pressures are required to keep the obstructive apneas from occurring, a Bi-level machine allows a person to exhale more comfortably and to adapt more easily to the use of the pressure.
There are additional types of pressure sources which have been developed for very specific medical needs. These pressure machines have been designed to support breathing, not just to keep airways open and prevent apnea. These machines adopt some of the techniques employed in hospital critical care units that provide artificial ventilation to extremely ill individuals. The technique of using external air pressure to artificially breathe for a person is over fifty years old. Modifications of the positive air pressure machines with specific upgraded functions, both CPAP and Bi-level, can provide for some limited types of artificial ventilation support.
The pressures generated by the CPAP and Bi-level machines are determined by your physician and the machine is set to deliver those pressures.
Pressure Source Special Features
There are several special features available in many, if not most, pressure machines.The most common feature is a ‘pressure ramp.’ The ramp feature allows the machine to gradually increase the pressure delivered over a period of five to forty-five minutes. This permits the person to fall asleep at a low pressure. Then it is slowly increased to the set therapeutic pressure. It is particularly helpful when someone first starts using CPAP.
‘Auto altitude adjustment’ will adjust the pressure the machine generates so that it is appropriate for the altitude were it is being used. The pressure machine is generating air pressure which is set to deliver pressure a certain level above the atmospheric pressure. The atmospheric pressure changes with the altitude, so if you travel to the mountains from the seashore, the pressure of the machine should be adjusted. All machines are manually adjustable, but the auto altitude adjustment feature makes the changes when a machine’s location and altitude changes.
‘Memory card’ options are available for many machines. The card records certain information on the machine’s performance and can be ‘read’ by your physician. The information explains how the machine is being used and what happens while it is used. It is particularly helpful if the person is having problems. The problems can often be identified and correted from the information on the card. This may help one avoid another sleep test.
‘End exhalation pressure reduction’ is a relatively new feature that is available on some pressure machines. The machines equipped with this feature allow for a rapid, brief drop in the set pressure during exhalation. Respironics developed C-Flex™ technology, the first commercially available form of this feature. CPAP with C-Flex delivers a set pressure, such as 10cm, upon inhalation. However, the exhalation pressure may be lowered by 1, 2, or 3cm to increase patient comfort. For instance, if the CPAP setting is 10cm and the C-Flex setting is 3cm, the person will always inhale at 10cm and exhale at 7cm. ResMed has a similar product available that they call EPR™. The settings on the different machines with exhalation pressure reduction work the same, although there are some technical differences.
THE INTERFACE
The second component involved in PAP therapy is the interface, also called a mask. This is the component that contains the pressurized air for the person to breathe. A single tube connects the pressure machine to the interface. The mask is designed to provide air under positive pressure by forming a seal at the nose or at both the nose and mouth. As the air is pumped under pressure to the mask, it is held under positive pressure while the person breathes. There are five basic mask designs available: the nasal mask, the nasal pillows mask, the full-face mask, the hybrid mask, and the oral mask. For each of these designs there are many different styles available.
The nasal mask covers the nose and a seal is formed against the face. An example of a nasal mask is the Respironics Comfort Gel™. The nasal pillows mask rests just inside the nostrils and create a seal at the outer edge of each nostril. The ResMed Swift II™ is an example of a nasal pillows type of mask.
There are many people who breathe through their mouths when asleep for a variety of reasons. Some may have a chronic nasal obstruction and some people have learned to breathe through their mouths as a response to sleep apnea itself. Since the mouth needs to be closed when using a nasal mask to maintain the therapeutic pressure, there are two solutions. First, a person with a nasal mask may add a chin strap to aid in keeping the mouth closed. The other alternative is to use a full-face mask. The full-face mask is designed to cover both the nose and mouth while maintaining an adequate seal. The newest type of full-face mask is a combination of mouth cushion and nasal pillows. The Fisher & Paykel FlexiFit 432™ and ResMed Liberty™ are examples of a full-face and full-face hybrid mask.
The final mask type is an oral mask. Fisher & Paykel’s Oracle™ is the only variety available on the market. This mask is not used very often, but may be of benefit to a person who has severe skin reactions to the materials of some masks, or who has severe airflow obstruction through the nose.
HEATED HUMIDIFICATION
Our respiratory tract has to be able to adapt to many types of air as we move from season to season and travel to many places. One major factor that affects our respiratory system is the humidity of the air we breathe. Ideally, our air would be of a constant temperature and humidity, but that just never occurs. When air is breathed through a CPAP machine, humidity can be added to the air making the positive air pressure more easily tolerated. As a result, humidifiers are available for almost all of the commercially available CPAP machines.
The addition of extra humidity to the air supplied through the CPAP machine improves the person’s ability to use positive air pressure. The units, a water reservoir and heater, are generally connected directly to the pressure source. The heater is designed to heat the water just enough to add humidity to the air. The heating scale is a simple range from ‘off’ to ‘warm.’ The setting and the ideal amount of humidity is that which the person using the system finds comfortable.
SELF REGULATING POSITIVE AIRWAY PRESSURE THERAPY
The two main types of positive airway pressure, CPAP and Bi-level, were described above. Within the categories of CPAP and Bi-level there are more specialized forms of PAP as well.
Another type of pressure therapy machine is the Auto-Titration machine. Auto-titration means that the machine will estimate and deliver the amount of pressure needed at each breath. The machine has a pressure range from low to high and it will deliver pressure at any level within that range as needed to prevent the obstructive events. The sensors in the machine are designed to identify the apnea events and adjust the pressure to correct the problems. These machines are of most value when the physician cannot determine the ideal treatment pressure.
Auto-Titration machines are available in both the CPAP and Bi-Level forms of positive airway pressure machines.
